Copyright 2024
Medical Security Card Company, LLC
All Rights Reserved
WellRx will never sell your personal information. Period. By signing up I agree to WellRx's terms of use and privacy policy.
By Jillian Foglesong Stabile, MD
April 12, 2024
Anytime you experience abnormalities with your bowels, whether it is constipation, diarrhea, gas, or pain, it can be disturbing and concerning. You may be worried about the symptoms you’re experiencing and wonder if they could be warning signs of some more severe problem. Chronic diarrhea, in particular, can be very disruptive. If you’re having to plan your day around rushing to the bathroom, you may wonder what options you have for the management of your chronic diarrhea.
Chronic diarrhea is defined as a decrease in the consistency of the stool for at least four weeks. It affects up to five percent of the population. Any of several hundred different conditions can cause chronic diarrhea, which makes the diagnosis and management of the condition challenging.
Chronic diarrhea can generally be categorized into 3 basic categories: watery, fatty, and inflammatory. These 3 categories often overlap.
Watery diarrhea comes in a few sub-categories. Osmotic diarrhea occurs when the bowels retain water because there are poorly absorbed substances present. Secretory diarrhea occurs because of reduced water absorption. Functional diarrhea is when the colon is overactive. Secretory diarrhea is associated with significantly higher volumes of stool and continues despite fasting and occurs at night. Functional diarrhea is generally associated with smaller stool volumes and no diarrhea at night.
Fatty diarrhea is generally associated with malabsorption. Malabsorptive diarrhea is associated with diarrhea, weight loss, and bulky stools. The stool is generally foul-smelling and oily. It may even float and be difficult to flush. The diarrhea may be explosive, associated with gas, or cause abdominal bloating. The weight loss associated with malabsorptive diarrhea is generally due to problems with the digestion of food and absorption of nutrients. This may be due to inadequate amounts of digestive enzymes, an imbalance of acid in the stomach, or bacterial overgrowth in the small intestine.
Inflammatory diarrhea is frequently bloody. The diarrhea is usually frequent, small in volume, and associated with fever or abdominal pain. Certain inflammatory markers such as white blood cells (leukocytes) or associated proteins such as calprotectin or lactoferrin may be seen in the stool on testing. Other inflammatory markers may be seen in the blood in patients with inflammatory diarrhea.
Some factors may be associated with an increased risk of developing chronic diarrhea. One study found that self-reported food sensitivities and increased stress were both associated with increased chronic diarrhea. Higher levels of education and being of female gender were associated with less likelihood of developing chronic diarrhea. Some specific causes of chronic diarrhea may have a genetic link, which means that a family history of the disease may increase your risk.
Chronic diarrhea is associated with a large number of conditions. Some of these conditions are things that you can modify yourself, but others may require medication to control the symptoms.
Many foods are associated with chronic diarrhea. Sugars, especially those that are poorly absorbed, are frequently associated with chronic diarrhea. Fructose is the most common natural sugar associated with diarrhea while artificial sweeteners such as sorbitol, mannitol, and xylitol are also common culprits.
For many people, dairy foods are associated with diarrhea. It is common for people to lack the lactose enzyme that breaks down milk sugars, which leads to chronic diarrhea. Gluten is another common culprit for people with gluten sensitivity or celiac disease. Other people may be sensitive to fried, fatty, or spicy foods. Caffeine increases intestinal motility and can cause diarrhea as well.
Several classes of medications are also associated with diarrhea. Nonsteroidal anti-inflammatory drugs, certain types of medications for reflux, antibiotics, herbal supplements, antidepressants, some diabetic drugs, some blood pressure medications, and chemotherapy are all associated with diarrhea that can become chronic. High doses of some vitamins or minerals may also be to blame. If you think your medications may be causing your diarrhea, make sure to talk with your healthcare provider before stopping any medication.
The osmotic form of chronic watery diarrhea can be associated with certain types of laxatives such as lactulose or magnesium citrate. Lactose intolerance also causes chronic diarrhea associated with the consumption of milk or other lactose-containing foods. Irritable bowel syndrome with diarrhea is also associated with chronic watery diarrhea.
Malabsorption-related diarrhea can be caused by several conditions:
Inflammatory diarrhea can be infectious and associated with proteins, blood, or pus. Diverticulitis, inflammatory bowel disease such as Crohn’s, ulcerative colitis, collagenous colitis or lymphocytic colitis, or infections with organisms such as shigella, salmonella, or campylobacter are associated with inflammatory diarrhea. Several viral and parasitic diseases are also associated with chronic diarrhea. In some cases, colorectal cancer may be associated with chronic diarrhea. Anything that causes damage or inflammation in the colon can cause symptoms.
The first step in the diagnosis of any disease is a good history and physical examination. Bloodwork can also help make the diagnosis. Frequently, your healthcare provider may recommend a complete blood count, metabolic panel, or labs to rule out celiac disease. If you are experiencing alarming symptoms such as blood or weight loss, additional testing may be recommended. This may include stool studies for infection or inflammatory markers. If inflammatory bowel disease or colon cancer is suspected, the provider may order a colonoscopy to evaluate the colon lining for inflammation. Certain conditions such as microscopic colitis and celiac disease require biopsies to evaluate the colon lining.
Irritable bowel syndrome is a diagnosis of exclusion meaning that there is not a specific test to make the diagnosis. It is based on clinical history and the lack of other diagnoses.
The approach to managing chronic diarrhea depends on the cause of the symptoms. If your chronic diarrhea is associated with food, then avoiding the foods that cause your symptoms is the first step. Patients who have celiac disease must adhere to a very strict gluten-free diet. Staying on top of fluids to prevent dehydration, eating low-fiber foods, and avoiding overeating can all help manage the symptoms. In some cases, such as watery diarrhea, increasing fiber may actually be helpful as it absorbs water and bulks up the stool.
Infectious diarrhea can be avoided by properly cooking food, cleaning surfaces to prevent contamination, and washing your hands frequently.
Over-the-counter medications for chronic diarrhea include antidiarrheal medications such as bismuth or loperamide slow down the transit of matter through the colon and can slow diarrhea. These should be used with caution and under the guidance of a healthcare provider because using antidiarrheals in the case of infections can slow the clearing of the infection and increase the risk of complications.
Probiotic medications can help restore the balance of good bacteria in the colon.
Prescription medication choices depend on the cause of the diarrhea. If the diarrhea is due to excess bile acids in the colon, then a medication to bind bile acids is helpful. Some anti-nausea medications such as ondansetron have also been shown to slow colon transit.
Antispasmodic medications can help control pain and chronic diarrhea in patients with irritable bowel syndrome. Some antibiotics such as rifaximin are also used for IBS with diarrhea.
Some types of intestinal infections can be treated with antibiotics. Clostridium difficile infection, in particular, may require multiple or prolonged courses of antibiotics to prevent recurrence.
Chron’s and ulcerative colitis can be treated with steroids or a class of medications called aminosalicylates. In some cases, medications to suppress the immune system are needed. Several classes of medications can be used to manage the symptoms. Azathioprine, mercaptopurine, and methotrexate are medications used for many different conditions that are also used in inflammatory bowel disease. Newer agents that suppress the immune system such as Xeljanz, Rinvoq, or Zeposia are all pills that modulate the immune system and treat inflammatory bowel disease. Several intravenous infusions can also treat inflammatory bowel disease.
Microscopic colitis can be controlled, though medication isn’t a cure. Treatment is generally aimed at controlling the symptoms. Antidiarrheals are frequently used and may be enough to control symptoms for some patients. If these medications are not enough to control the symptoms, then the next step is generally to add a medication such as cholestyramine or bismuth sulfate. Other therapies such as steroids are used in situations when other medications aren’t effective at controlling the symptoms.
Monitoring symptoms and discussing your concerns with your doctor is one of the most important things that you can do. If your doctor has recommended medication for your chronic diarrhea, consider using our WellRx prescription discount card. Some people save a little. Some people save a lot and prices vary across zip codes. Even pharmacies across the street from each other can have huge price differences! ScriptSave has been helping consumers save on their prescriptions for 25 years.
Dr. Foglesong Stabile is a board-certified Family Physician who enjoys full scope Family Medicine, including obstetrics, women’s health, and endoscopy, as well as caring for children and adults of all ages. She also teaches the family medicine clerkship for Pacific Northwest University of Health Sciences.
References:
https://www.aafp.org/pubs/afp/issues/2011/1115/p1119.html
https://www.merckmanuals.com/home/digestive-disorders/malabsorption/overview-of-malabsorption
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538472/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2946219/
https://my.clevelandclinic.org/health/diseases/24311-chronic-diarrhea
https://www.ncbi.nlm.nih.gov/books/NBK544337/
https://www.health.harvard.edu/diseases-and-conditions/is-something-in-your-diet-causing-diarrhea
https://www.ncbi.nlm.nih.gov/books/NBK414/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10321507/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4755466/
https://www.aafp.org/pubs/afp/issues/2020/0415/p472.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4641856/

For your convenience, use the ScriptSave® WellRx mobile app. Now savings are well in hand, right at the pharmacy counter. Save on your family's prescription medicines.
Learn More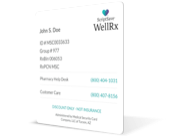
Your choice. Get a ScriptSave WellRx Savings Card. Or Download the free mobile app from the App Store or Google Play Store
Get A Card
ScriptSave WellRx Grocery Guidance leverages leading-edge nutritional data science to help you know which food products on your grocery store shelf are truly good for YOU.
Healthy Foods For YouTags:

October 23, 2024

May 07, 2024

April 04, 2024
You need to log into the site to use this feature
This feature requires registration. Sign up or log in to your free WellRx account to gain access to this and other tools to help make managing your medications and wellness easier.
Benefits Include:
This feature requires registration. Sign up or log in to your free WellRx account to gain access to this and other tools to help make managing your medications and wellness easier.
Benefits Include:
You will be redirected to your program in 5 seconds.
Our Terms and Conditions and Privacy Policy have recently been updated.
By declining you will be logged out of your account